The magic bullet: heat-seeking drugs
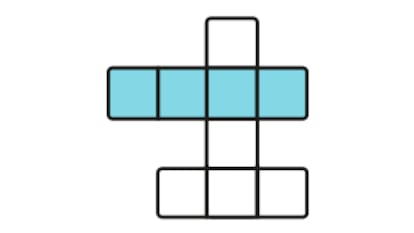
The magic bullet. Scientists in the sixties believed they had discovered this when they prepared small bubbles composed of natural components of the cell membrane. These artificial vesicles, named liposomes, can be made simply by mixing natural lipid molecules. This leads to liposomes with an aqueous interior forming spontaneously. Drugs can easily be incorporated in the interior of the liposomes, raising the possibility that drugs can be transported specifically to their target. Such a drug delivery strategy would improve therapy, especially in cancer treatment where the patients' life quality is significantly compromised by the severe systemic side effects of conventional treatment.
In fact, the optimistic view of early researchers has not been translated into clinical practice as yet. More than 40 years later, only a few liposomal drugs are approved. However, none of these have shown an increased antitumor effectivity compared to free drug and approval was granted due to a reduction in specific organ toxicity only. The main cause for the initial failure of liposomes was the unsolved problem of triggered drug release. The liposomes have to be chemically stabilized in order to prevent rapid degradation after intravenous application. This leads to liposomes with very long plasma circulation half lives. Since the tumor vessels - but not the surrounding, healthy vessels - are leaky, the circulating liposomal drugs passively leak into and hence accumulate in the tumor tissue. However, despite this accumulation at the tumor target, there is not sufficient drug release out of the carrier system.
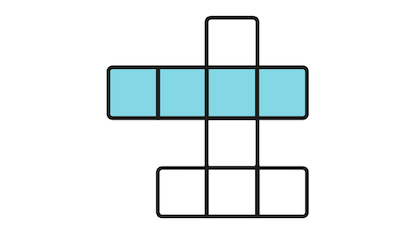
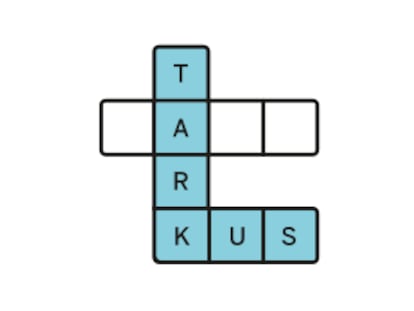
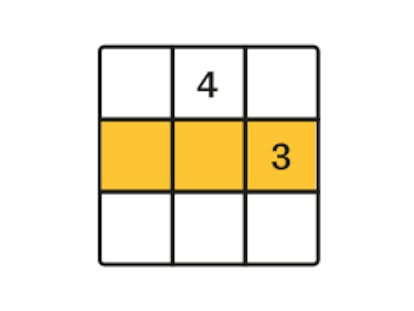
A method is required to trigger release of the active drug from its liposome carrier. In 1978, the principle using heat was first established. Liposomes are synthesized from phospholipids, which have a unique chemical structure that allows a change in aggregate state from solid to fluid at a distinct temperature. This results in liposomes becoming "leaky" when increasing the body temperature from 37 to 41 °C in the target area, in theory releasing the drug at the target location. It has taken more than 20 years for such temperature-sensitive liposomes to be developed and tested successfully in animals. However, these liposomes - designed at Duke University in the USA - suffer from insufficient stability at body temperature, resulting in a significant loss of their payload before reaching the target.
Why has there been such a huge delay in clinical development of this novel treatment strategy? There are two major reasons: first, the availability of the sophisticated chemistry involved, and, second the development of clinical hyperthermia. A lucky coincidence enabled me to find access to the solution of this problem during my career. During my thesis work with Prof. Eibl at the Max Planck Institute for Biophysical Chemistry in Goettingen, Germany, I learned about the nature of phospholipids and that specific modification of single atoms in their structure can lead to novel biological properties. After finishing my thesis, I moved to the Ludwig-Maximillians University in Munich to start a residency in hematology/ oncology. Here I met Prof. Issels, who specialises in clinical hyperthermia using electromagnetic deep heating devices. Influenced by the enthusiasm of both scientists, I had the feeling that this would be the ideal situation to further develop thermosensitive liposomes for the targeted treatment of cancer patients.
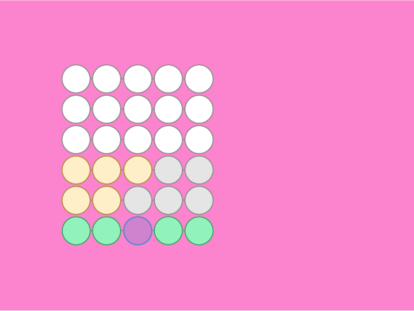
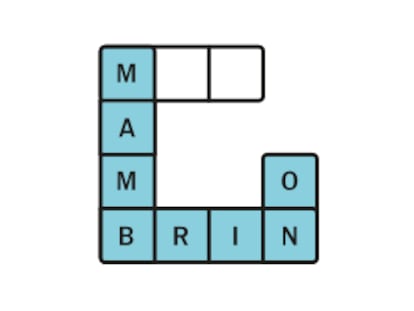
Excited by the idea of targeted drug therapy by first encapsulating the drug within a liposome and second triggering its release in the tumor by heating, I started my own research group dedicated to this idea. Based on novel synthetic phospholipids from Prof. Eibl, we have developed a system that is adapted to the clinical need of the patient. First, our liposomes are stable at 37 °C in the blood stream and circulate throughout the whole body without unspecific accumulation in normal tissue during the first two hours. Second, after mild heating the drug is released within a few seconds. The released drug reaches the tumor via the natural blood vessels at a concentration more than 10-fold higher than that in the blood. In animal experiments, this leads to a complete tumor regression compared to almost no effect being observed for the free drug or for conventional liposomes.
It is fantastic for me as a physician to develop a new drug from bench to bedside and thereby bring together technologies which otherwise would never have met. This new treatment method will allow the treatment of advanced tumours by increased local efficiency and decreased systemic toxicity. Our vision is obvious: having a new temperature-sensitive liposome approved and in widespread use for cancer treatment. In addition, novel treatment options are on the horizon combining the simultaneous encapsulation of MRI contrast agent where MRI-controlled drug release allows treatment guidance in real time. Pushing these developments forward in addition to the regular clinical work requires an intense time commitment from me. Luckily, my wife shares my enthusiasm for clinical research and the potential benefit it holds for patients.